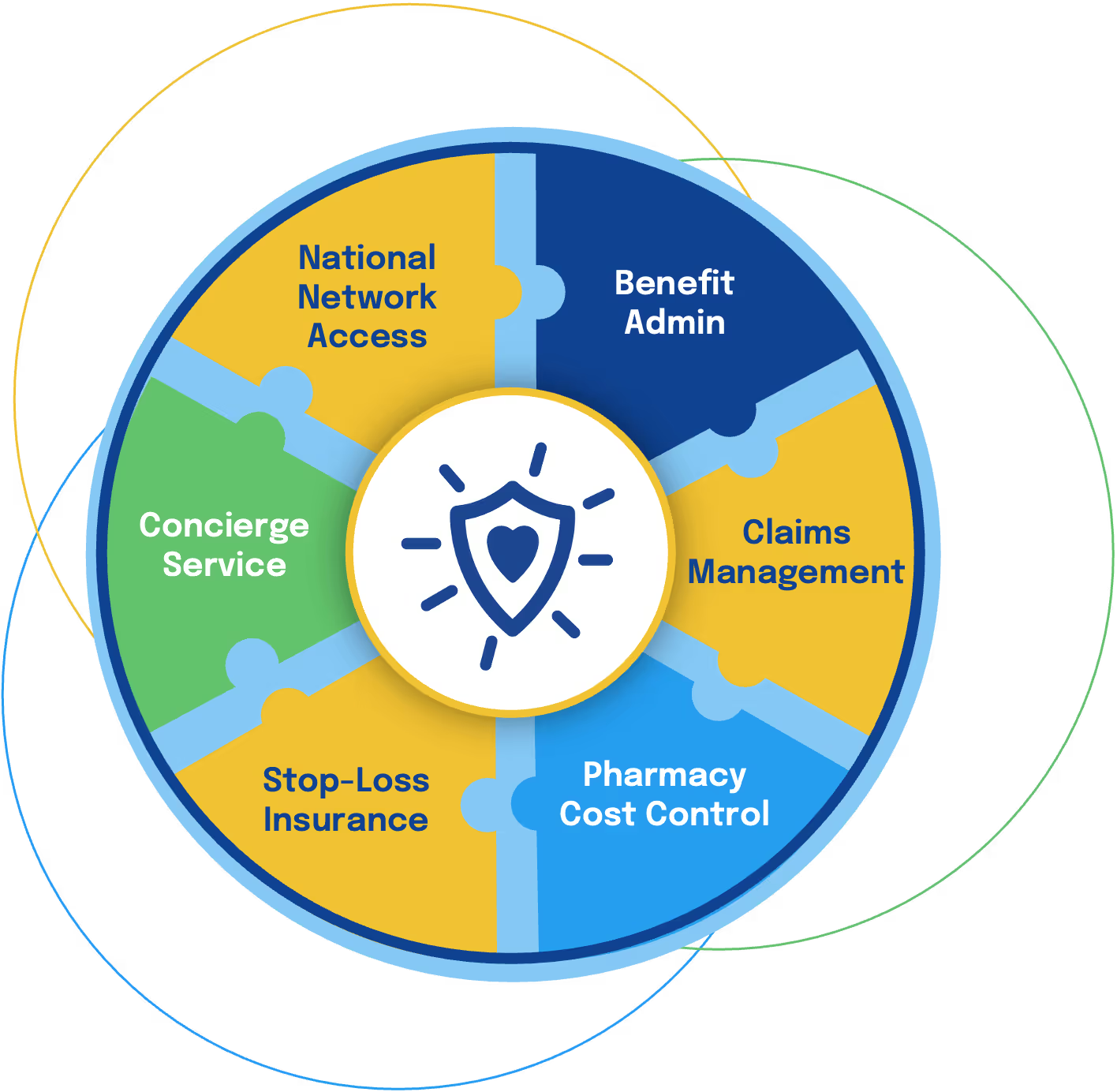
ProVision Health leads and coordinates every aspect of our
cost-containment strategy —from advanced analytics to specialty drug management — delivering integrated, seamless, and cost-effective healthcare solutions.
Optimizing plan performance requires broad in-network options and strong discounts. Our claims platform enhances PPO networks, cutting costs, ensuring fair provider compensation, and offering nationwide access through the nations most trusted PPO network.
Key Benefits:
- Over 1.7 million facilities and practitioners across all 50 states, ensuring coverage where it’s needed most. The scope of the network maximizes provider availability while reducing out-of-network claims and enhancing member satisfaction.

Comprehensive benefits administration focused on maximizing plan performance and reducing costs through advanced claims management and experienced personnel.
Key Benefits:
- Plan Design: Tailored plans to reduce over-utilization and financial strain for optimal value.
- Experienced Team: Staff avg.15+ years of expertise to tackle complex healthcare needs.
- Data-Driven Insights: Analytics reveal high-cost claims, trends, and utilization for smarter decisions.

AI-driven techniques and experienced professionals who detect waste, fraud, and inefficiency in real-time.
Key Benefits:
- Prepayment accuracy, post-payment recovery, custom analytics, and reporting.
- Delivers ~ Consistently outperforms expected claims as determined by the Program actuaries.
- Uses varied claims mitigation strategies.
- Implements strong cost containment.

Reduced pharmacy costs by up to 30% through strategic partnerships, analytics, and targeted cost-containment programs.
Key Benefits:
- Transparent Reporting: All RX rebates returned to the plan sponsor.
- Exceptional Formulary Management
- Innovative PBM Partnerships
- Specialty Drug Cost Containment Programs

Comprehensive protection against high-cost claims with access to industry-leading insurers.
Highlights
- Lower premiums and optimized terms for significant financial savings.
- Mitigates company risk or exposure to catastrophic claims.
- ProVision plans are rated with lower premiums and favorable terms than tradition plans.
- The Company We Keep: Gerber Life & Nationwide.
- Proven claims experience, effective tools.
- Offers unmatched discounted rates.

Dedicated support for finding in-network providers, managing claims, and clarifying benefits.
Key Benefits:
- Single point of contact - dedicated assigned customer service representative for the duration of the claim.
- Increased satisfaction.
- Minimized healthcare navigation hassles
- US based service team

Our program's collective strengths—independent administration, innovative plan design, superior analytics, cost efficiency, and an enhanced stop-loss program—offer a next-generation Healthcare program.
Comprehensive Program: Integrates all key components (benefits admin, claims analytics, concierge services, pharmacy cost containment, stop-loss insurance, and network partnerships)
Transparency and Cost Control: The program offers complete transparency in pricing and claims processing, with a focus on controlling costs across all areas.
Member Advocacy: Prioritizes the needs of members, ensuring they receive the best possible service and outcomes.
Leadership and Experience: With offices in New York, Florida, and California, we bring the expertise and experience needed to deliver a cohesive program that outperforms traditional models.
Key Partnerships: Our ablity to partner with industry leading companies throughout the healthcare space creates a solution that works within the existing system while advancing and improving outcome.




